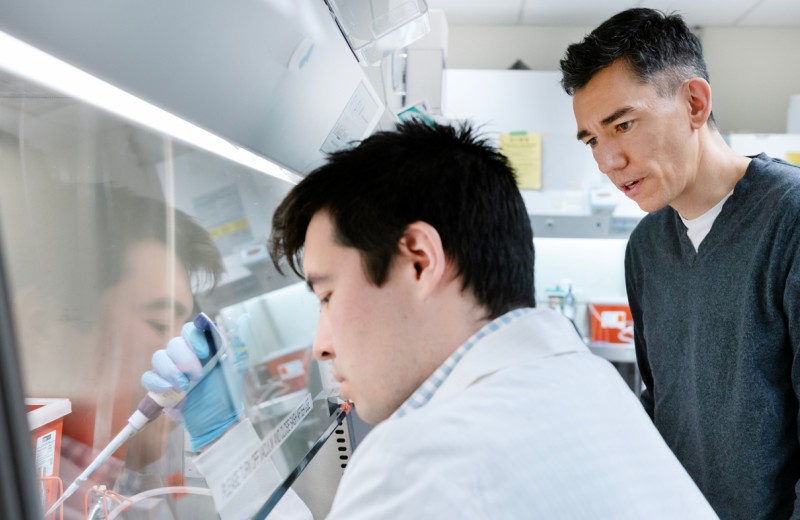
Ken Nakamura, MD, PhD, developed new tests to accurately measure brain’s energy supply, which is essential for understanding how impairments in the system cause neurodegeneration. [Photo: Chris Goodfellow, Gladstone Institutes]
A new study from the Gladstone Institutes shows for the first time that impairments in mitochondria—the brain’s cellular power plants—can deplete cellular energy levels and cause neuronal dysfunction in a model of neurodegenerative disease.
A link between mitochondria, energy failure, and neurodegeneration has long been hypothesized. However, no previous studies were able to comprehensively investigate the connection because sufficiently sensitive tests, or assays, were not available to measure ATP (the energy unit of the cell that is generated by mitochondria) in individual neurons.
In the current study, which was chosen as the Paper of the Week in the Journal of Biological Chemistry, the scientists created novel assays to more accurately measure the brain’s energy production. Using a model of Leigh’s disease, a genetically inherited neurodegenerative disorder that affects mitochondria, the researchers tested energy levels in neurons using the new assays. They found that the genetic mutation associated with Leigh’s disease compromised ATP levels, and this reduction of ATP was enough to cause significant cellular dysfunction.
“It was always assumed that defects in mitochondria would result in a depletion of energy levels, which would be toxic to neurons,” says first author Divya Pathak, PhD, a postdoctoral fellow in the Gladstone Institute of Neurological Disease. “But no one had been able to prove this because the necessary assays were not available. Now that we’ve demonstrated the link between impaired mitochondria, a loss of ATP, and neuronal dysfunction, the next step is to see if this connection holds true in conditions like Parkinson’s disease and Alzheimer’s disease.”
Applying their new assay in healthy neurons, the researchers also determined the energy threshold needed to support synaptic vesicle cycling—the process by which brain cells release neurotransmitters to communicate with each other. The scientists blocked glycolysis, another way that cells make ATP, so that the cells had to rely solely on their mitochondria for energy. This allowed the researchers to more accurately assess the contribution of mitochondrial ATP to different steps in the cycle, and how this process goes awry when mitochondria malfunction.
From this exploration, the scientists revealed that bringing the vesicles back up into the cell after they have released their neurotransmitters is the most energy-demanding process. Indeed, in the model of Leigh’s disease, the cells did not have enough ATP to complete this step.
The researchers also compared energy levels in boutons—the docks from which neurotransmitters are shipped—with and without mitochondria. Remarkably, there was no difference in energy levels between the two, and both types of boutons had sufficient ATP to support synaptic vesicle cycling. From this, the scientists concluded that under normal conditions, ATP diffuses rapidly from boutons with mitochondria to those without, so that even those boutons lacking mitochondria have sufficient energy to function under normal conditions. They note it will be important to determine if boutons lacking mitochondria will still be able to function properly in diseases that disrupt the distribution of mitochondria.
Senior author Ken Nakamura, MD, PhD, an assistant investigator at the Gladstone Institute of Neurological Disease, says that conducting this research in both healthy and diseased cells is essential for interpreting the findings. “We really need to understand the basics of cell biology in a normal setting in order to comprehend changes in disease,” he explains. “It’s worth taking the time to study these underlying biological processes so that we can identify the best therapeutic targets for neurodegenerative disorders.”
Other investigators on the study include Lauren Shields, Bryce Mendelsohn, Dominik Haddad, Wei Lin, and Hwajin Kim from the Gladstone Institutes; Akos Gerencser and Martin Brand from the Buck Institute for Research on Aging; and Robert Edwards from the University of California San Francisco.
The study was supported by grants from the National Institutes of Health, the Burroughs Wellcome Fund, the National Science Foundation, the Pediatric Scientist Development Program and from the Betty Brown Family, and the Joan and David Traitel Family Trust.
Support Our COVID-19 Research Efforts
Gladstone scientists are moving quickly to respond to the coronavirus outbreak. Help us end this pandemic.
Cellular Clean Energy: Can Mitochondria Make More Energy Without Collateral Damage?
Cellular Clean Energy: Can Mitochondria Make More Energy Without Collateral Damage?
New research from Gladstone may help in the development of new therapies that target the problem of cellular energy failure—a hallmark of Parkinson’s, Alzheimer’s, and aging in general
News Release Research (Publication) Alzheimer’s Disease Parkinson’s Disease Neurological Disease Nakamura Lab CRISPR/Gene EditingSugar Rush: Scientists Discover Key Role of Glucose in Brain Activity
Sugar Rush: Scientists Discover Key Role of Glucose in Brain Activity
New details on how healthy neurons metabolize glucose have implications for understanding neurodegenerative diseases
News Release Research (Publication) Parkinson’s Disease Alzheimer’s Disease Neurological Disease Nakamura LabRecycling a Cell’s Energy Centers to Ward Off Parkinson’s Disease
Recycling a Cell’s Energy Centers to Ward Off Parkinson’s Disease
Gladstone researchers tracked mitochondria inside brain cells and uncovered a new recycling pathway that may be linked to disease
News Release Research (Publication) Parkinson’s Disease Neurological Disease Nakamura Lab